The Synergy of Ketamine and Therapy for Emotional Healing: An Austin Therapist's Perspective
Maximal Benefits of Ketamine through Therapy with Andrea Marquez LCSW
In the heart of Austin, Texas and a few hours north in Dallas-Fort Worth patients arrive at Heading clinics to receive a groundbreaking approach to mental health and the treatment of depression, anxiety, and PTSD – Ketamine therapy. Ketamine Therapy, known for its association with psychedelic substances, has emerged as a beacon of hope for individuals battling mood disorders that have not been helped well enough, or at all, by traditionally prescribed first-line treatments. What sets this therapy apart is how its effects on the brain can directly integrate with the benefits of counseling, creating a dynamic duo that optimizes treatment for those seeking profound emotional healing.
Most often patients in Heading’s care receive treatments in the form of Intramuscular Ketamine or in a nasal-spray medication called Spravato®. Patients will physically come in for Ketamine in Austin or Ketamine in Dallas to a Heading clinic. Ketamine treatment is a series of treatments over several weeks, and the safety, comfort, and expert support of in center treatments makes the choice to have in-person treatment well worth the visit.
Conveniently, in between treatments patients are often paired with a therapist that sees the patient virtually. Combining virtual therapy appointments optimizes the benefits of the in-center treatment with the transformative change that can come from working with a licensed therapist who understands the healing potential of Ketamine, and the unique effects it has on the brain. This article shares the perspective of one of Heading’s therapists who often treats patients who are also receiving Ketamine or Spravato® in the center.
Meet Andrea Marquez, LCSW, a respected therapist and supervisor at Heading, who has been at the forefront of this innovative approach, combining the transformative power of Ketamine treatments with the healing potential of therapy. Andrea’s dedication to her patients’ well-being has led her to explore the untapped potential of neuroplasticity and the behavioral change that therapy can evoke in conjunction with Ketamine’s effects on the brain.

Groundbreaking Synergy: Therapy and Ketamine Unite
When asked to provide insight into the benefit of combination therapy and ketamine Andrea explained how the two healing modalities complement each other, creating a well-rounded experience for her patients. “Therapy combined with interventional treatment has been helpful in keeping patients engaged in treatment and gives them the ability to check in on their concerns and experiences,” she shared.
Still, some patients are nervous about Ketamine, associating it with its illicit use and abuse as a street or party drug. Andrea understands their nerves and feels the combination of ketamine and therapy can calm these fears, and enhance safety and efficacy, “By providing a supportive environment, therapy helps destigmatize the use of Ketamine and empowers patients to make sense of their unique journey with the treatment and understand its usefulness.”
Neuroplasticity Unleashed: Ketamine Opens the Door
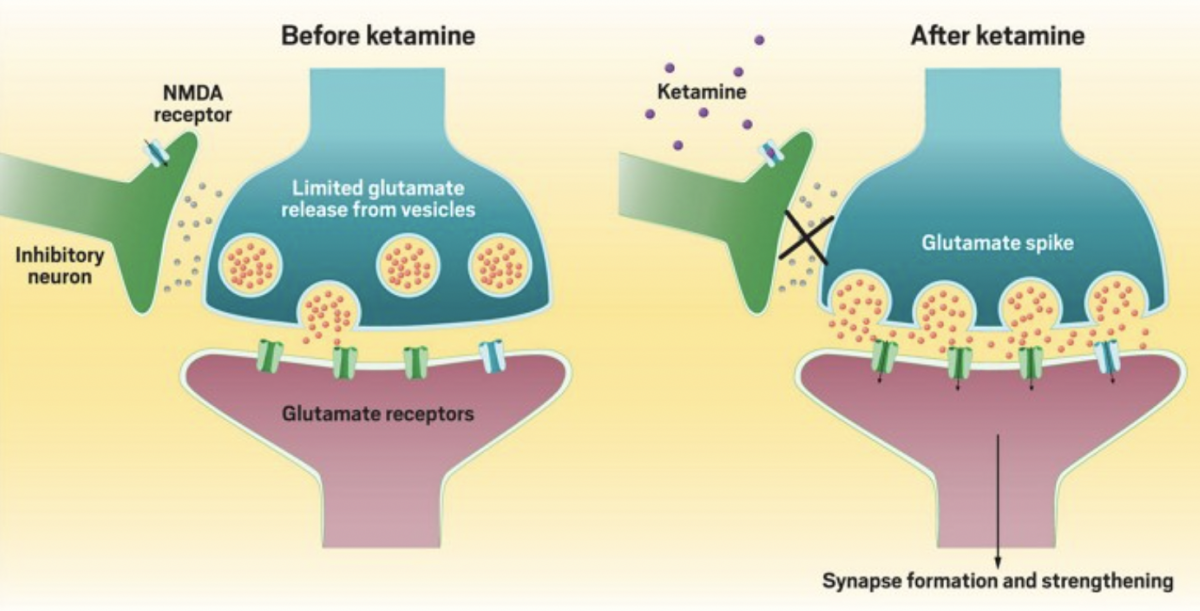
Andrea’s expertise in mental health and her understanding of neuroplasticity have led her to recognize the window of opportunity that Ketamine treatments offer. “Ketamine treatments place the brain in a unique state making it more receptive to change,” Andrea explained.
It was an old belief that the physical structure of the brain became relatively unchangeable after a certain stage of development. Now scientists, psychiatrists, and therapists who are experts on the brain and thought processes know that this is not true. The brain is capable of change and healing. This capability for change, or neuroplasticity, is key in changing long held habits. Ketamine heightens the neuroplastic state and in this heightened state patients have the potential to break free from negative thought patterns and establish new neural connections, creating lasting positive changes in their mental landscape.
Reinforcement and Resilience: Grounding and Mindfulness Techniques
Ketamine therapy, though safe with relatively low risk of adverse side effects, can still be experienced as quite intense. While technically a dissociative anesthetic Ketamine produces a brain and body experience that is often described as psychedelic.
Prior to treatment Andrea teaches patients grounding and mindfulness techniques they can use during sessions, providing patients with invaluable tools to navigate their emotional experiences. These techniques can be employed in Ketamine sessions and in every day life. “If I am able to meet with them before they get started, I teach them mindfulness exercises like a body scan, paced breathing, and self-soothing techniques,” Andrea explained.
Feeling comfortable, safe, and well cared can make treatment a positive experience. Deep breathing, mindfulness techniques, and body scanning exercises help soothe the nervous system helping the patient’s breath rate, and heart rate remain calm, and bring awareness to areas of physical tightness or tension so that the patient can more fully relax.
These techniques not only assist patients during their Ketamine treatments but also equip them to cope with intense emotions in their everyday lives, fostering resilience and emotional well-being.
Empowering Positive Change: Therapy and the Power of Thought Processes
As mentioned, Ketamine opens windows to review experiences and emotions in a new way, and establish new healthier connections. The benefits do not go away when the acute effects of the medication wear off. Instead, time in between Ketamine treatments offers a special period to address anything that’s come up.
Unlike self-employed techniques like journaling or reflection, both of which can be very helpful, taking the added step to meet with trained therapists during a ketamine treatment series offers deeper benefits. Licensed therapists, especially those who have worked with patients who are going through ketamine treatment, have skills, and experience to employ a variety of techniques that can be tailored to the patient’s case, and needs in the moment.
One of the key aspects of therapy in conjunction with Ketamine treatments is the opportunity to work on thought processes. Andrea pointed out, “[After a treatment] We look at what comes up and what connections they make. Then I have the patient tell me what will best support them, whether it is just to hold space for those thoughts and emotions or if it is something they want to change.” Through this collaborative exploration, patients gain insights into their thoughts and emotions, empowering them to embrace their emotional healing journey.
In summary, Andrea emphasized the immense potential of integrating therapy with Ketamine treatments. This well-rounded approach creates a powerful synergy, optimizing the benefits of both Ketamine’s effect on the brain and the emotional healing, mindset shifts, and behavior change that therapy facilitates.
“Integrating therapy with Ketamine treatments allows patients to experience a more comprehensive and holistic approach to healing,” Andrea concluded.
Taking the Next Step
Through her expert guidance, Andrea illuminates the untapped potential of neuroplasticity, the power of thought processes, and the significance of grounding and mindfulness techniques in this integrated treatment. As the world of mental health continues to evolve, the synergy of therapy and Ketamine promises hope and healing for those seeking relief from depression, anxiety, and PTSD.
If you are interested in learning more about Ketamine or Spravato® treatments to address major depression, anxiety, or PTSD email info@headinghealth.com to request a psychiatric consultation.
Want to find out if Heading is right for you?
Complete our consultation form and an intake specialist will get in touch.






 Unlike with most antidepressants, patients considering
Unlike with most antidepressants, patients considering 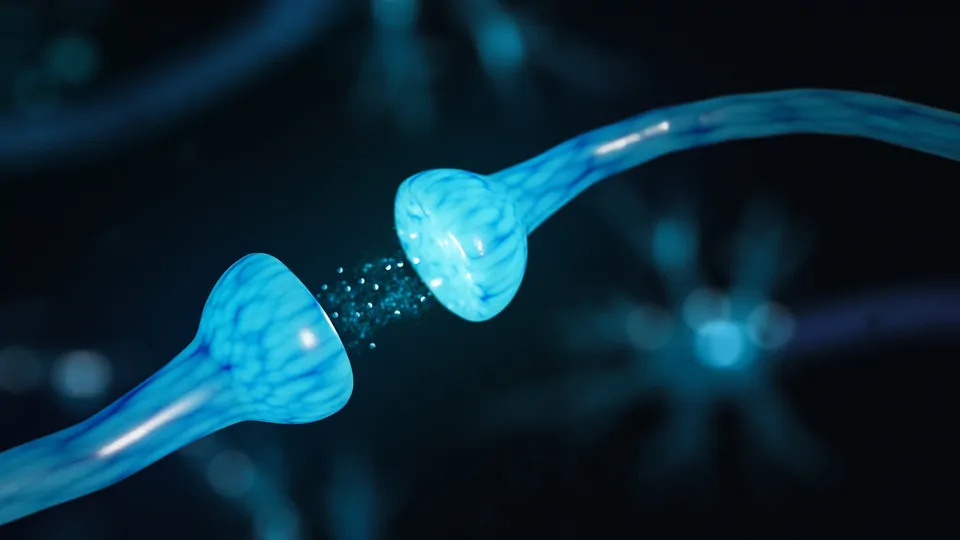
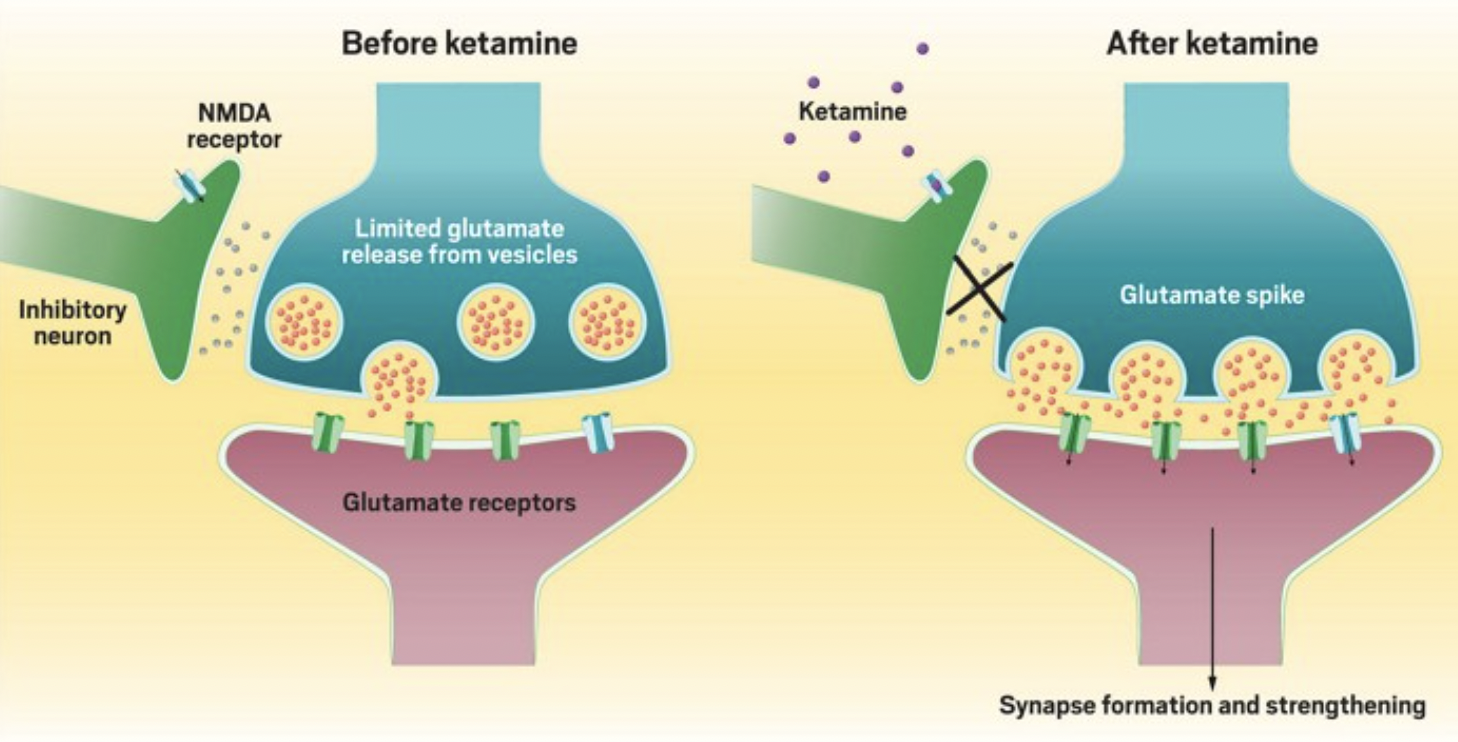
 changes are associated with better therapeutic outcomes. For example, ketamine appears to
changes are associated with better therapeutic outcomes. For example, ketamine appears to 





 I’ve always struggled to get myself to try new things. I like consistency and predictability, and new experiences get in the way of maintaining my desired level of stability.
I’ve always struggled to get myself to try new things. I like consistency and predictability, and new experiences get in the way of maintaining my desired level of stability.