Breaking the Stigma: The Truth About Mental Health Diagnoses
Whether you’ve just received a diagnosis or are curious about what it would mean if you got one, you likely have some questions about these mental health labels. Why are they so important? Do they mean your stress is permanent? How do they impact treatment?
We answer these questions and more below.

What Does a Mental Health Diagnosis Mean?
Mental health exists on a spectrum. We all experience stress and anxiety from time to time. For some people, it’s worse than others. According to Julie Isaacs, senior vice president of clinical operations and therapy here at Heading Health, stress, anxiety, and other states involved in mental health conditions are signs of a mental illness when they are disproportionate to the situation, persistent, cause a significant amount of distress, and interfere with your ability to function. For example, though everyone worries and experiences fear, this can turn into a generalized anxiety disorder (GAD) if it’s experienced for at least six months, tends to be excessive, and limits your ability to function (e.g., at your job or in your social relationships).
Why Diagnosis is Important
Though they can seem intimidating, mental health diagnoses are crucial components of the therapeutic process. Here’s why.
Gaining Insight
Receiving a mental health diagnosis can help explain why you’ve been struggling and anticipate what issues you may face going forward. For example, a diagnosis of post-traumatic stress disorder (PTSD) would explain why you have been experiencing nightmares, flashbacks, and panic attacks. Not only can this help you better navigate the condition in the future, but knowing PTSD has been the cause of your stress can alleviate any sense of guilt or shame you’ve been experiencing for having these symptoms in the first place.
Identifying the Proper Treatment
Different conditions respond better to different interventions. For example, while obsessive-compulsive disorder (OCD) can be addressed with selective serotonin reuptake inhibitors (SSRIs) such as Zoloft and Prozac, bipolar disorder is better handled by mood stabilizers, such as Depakote or Lithium.
By identifying your condition, your providers can make use of decades of research to offer you the most effective medications and therapeutic strategies.
Securing Insurance Coverage
Often, insurance companies will only cover a particular treatment if the patient has been diagnosed with a specific condition. For example, transcranial magnetic stimulation (TMS) is typically only covered for a limited set of conditions, such as treatment-resistant depression (TRD) and OCD.
Diagnosis and Stigma
Despite its benefits, diagnosis can come with a significant degree of stigma. People hold various negative beliefs about what it means to have a mental illness which can make seeking therapy or receiving a diagnosis a stressful, guilt-inducing process. For many, this can discourage them from seeking treatment in the first place. For example, a recent report found that 25 percent of those who did not seek help for their mental health cited stigma as the main reason why.
Myth Busting Common Misconceptions
Despite its benefits, diagnosis can come with a significant degree of stigma. People hold various negative beliefs about what it means to have a mental illness which can make seeking therapy or receiving a diagnosis a stressful, guilt-inducing process. For many, this can discourage them from seeking treatment in the first place. For example, a recent report found that 25 percent of those who did not seek help for their mental health cited stigma as the main reason why.
Myth #1: You Can’t Recover From a Mental Illness
Mental health conditions are often seen as life-long ailments with no hope of recovery.
Fact: A significant percentage of individuals with mental health conditions see substantial improvements in their symptoms after treatment. Many even experience remission, meaning they no longer show any signs of their initial illness.
Those who don’t respond to the first few treatments can find help from novel interventions. For example, studies have found a 69 percent response rate and 52 percent remission rate in patients treated with Spravato® (intranasal esketamine), which is FDA-approved for treatment-resistant depression. Similar results have been found for ketamine, and TMS.
Myth #2: Treatment is Scary
Ever since Once Flew Over The Cuckoo’s nest, mental health treatments have been poorly represented in movies and other forms of entertainment.
Fact: Treatment is typically a pretty mundane process. In many cases, patients can improve with talk therapy alone. Medications and other biological interventions have been refined over the past several decades and now provide more targeted side-effect-free relief.
Myth #3: Mental Illness is Rare
Stigma is likely directly responsible for this myth. The percentage of individuals with undiagnosed mental health conditions is almost certainly underestimated, as many are apprehensive about seeking help in the first place. Moreover, those who do get help may not be ready to talk about it with friends and family. This creates a false perception that mental illness is rare.
Fact: Mental illness is prevalent. According to the Centers for Disease Control and Prevention (CDC), more than 50 percent of people will be diagnosed with a mental illness at some point in their lifetime.
Myth #4: Only People with a Mental Illness Should See a Therapist
Since therapists treat individuals with mental health conditions, it’s natural to assume that you shouldn’t be in therapy unless you have a mental illness.
Fact: “The techniques and coping strategies therapists offer can help anyone dealing with stress and anxiety,” Patricia Hernandez, LCSW. “So whether your experiencing day-to-day stress, marital problems, or clinical depression, therapy can be a useful tool on your journey to mental wellness.”
Myth #5: Mental Health Problems Are a Sign of Weakness
Those who haven’t experienced a mental health condition themselves or don’t know anyone who has may not understand why someone might struggle to manage their stress and anxiety. As a result, mental illness is sometimes perceived to result from or be a sign of weakness.
Fact: There is no evidence to suggest that mental illness results from an internal weakness or lack of willpower.
“Individuals with mental illness are no less mentally tough than the average person,” shares Andrea Marquez, LCSW, an Austin, Texas-based therapist. In fact, the very opposite may be true. Managing a mental health condition requires strength, resilience, and a great deal of mental bravery.
Takeaway
Receiving a mental health diagnosis can be scary. With so many misconceptions regarding the nature of mental illness and its implications, it’s natural to feel concerned about the diagnosis you’ve received or the possibility of getting one were you to start therapy.
The reality is that diagnoses help both patients and providers understand their condition and offer the most effective treatments. While stigma still exists, its effects are waning, and by learning about what a mental health diagnosis does and doesn’t mean, you’re helping to paint a more accurate, optimistic picture of mental health.
Want to find out if Heading is right for you?
Complete our consultation form and an intake specialist will get in touch.













 Unlike with most antidepressants, patients considering
Unlike with most antidepressants, patients considering 
 Over the past few years, as safety precautions made many in-person services infeasible, we saw a dramatic and sustained rise in the use of telehealth services, including teletherapy and telepsychiatry. According to a
Over the past few years, as safety precautions made many in-person services infeasible, we saw a dramatic and sustained rise in the use of telehealth services, including teletherapy and telepsychiatry. According to a 

 Stress is generally seen as an undesirable state to be avoided whenever possible. It feels bad, can interfere with attention and productivity, and, when experienced chronically, may harm the body and lead to mental illnesses, including depression and generalized anxiety.
Stress is generally seen as an undesirable state to be avoided whenever possible. It feels bad, can interfere with attention and productivity, and, when experienced chronically, may harm the body and lead to mental illnesses, including depression and generalized anxiety. 
 Stress Can Enhance Your Memory
Stress Can Enhance Your Memory Memory is a good example of this. Animal studies show the brains of mice that underwent a stress test grew new neurons and performed better on learning and memory tests.
Memory is a good example of this. Animal studies show the brains of mice that underwent a stress test grew new neurons and performed better on learning and memory tests.  Perhaps more surprising than the beneficial effects of stress on the mind are its healing effects on the body. While we can get an intuitive sense of how stress might help us prepare for danger or feel extra motivated to complete tasks, it’s a little harder to see how it might benefit us at a biological level.
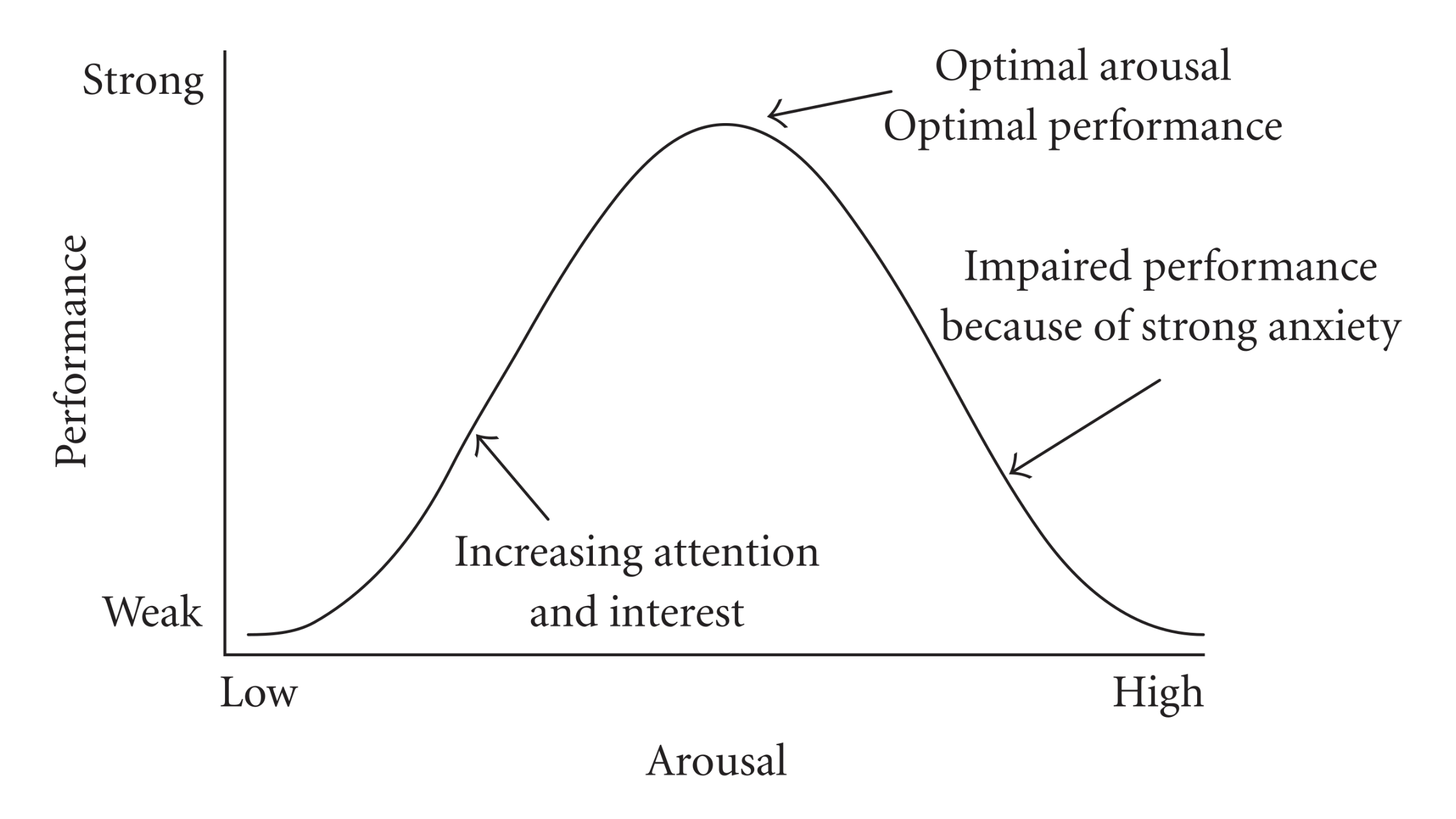
Perhaps more surprising than the beneficial effects of stress on the mind are its healing effects on the body. While we can get an intuitive sense of how stress might help us prepare for danger or feel extra motivated to complete tasks, it’s a little harder to see how it might benefit us at a biological level. As we learned from the Yerkes-Dodson Law, some stress is necessary for optimal performance. But how much is suitable for any person depends on various factors from skill level to personality to confidence. So how much is enough for you?
As we learned from the Yerkes-Dodson Law, some stress is necessary for optimal performance. But how much is suitable for any person depends on various factors from skill level to personality to confidence. So how much is enough for you? 

 both with and without medications had comparable improvements in their symptoms.
both with and without medications had comparable improvements in their symptoms. 
 Every year an estimated 800,000 U.S. adults make New Year’s resolutions in the hopes of improving their lives and developing healthier habits.
Every year an estimated 800,000 U.S. adults make New Year’s resolutions in the hopes of improving their lives and developing healthier habits. This is a perfectly normal reaction, and it’s important not to judge yourself if you’ve gone a little off course. “Guilt and shame will only serve to keep you from making progress,
This is a perfectly normal reaction, and it’s important not to judge yourself if you’ve gone a little off course. “Guilt and shame will only serve to keep you from making progress, Your journey to mental wellness will almost certainly require you to make some internal changes.
Your journey to mental wellness will almost certainly require you to make some internal changes.