Embarking on Your First Ketamine or Spravato® Treatment
If you’ve been prescribed ketamine or Spravato® for treatment-resistant depression, major anxiety disorder, PTSD, or another mental health challenge it’s normal to have a mixture of feelings and questions. Perhaps you are asking yourself
- “Do I need to have something in mind when I take the medication?”
- “What happens to my brain and body during treatment?”
- “Is there anything I should or shouldn’t do prior or after treatment?”
- “Are there safety concerns that I should consider?”
- “Am I going to ‘trip’?”
In this guide we will walk you through the first treatment process, and how this medication can support your health and healing.
We Assure Care and Safety.
Before Treatment
When you are receiving IM Ketamine or Spravato® at Heading you are in the care of doctors, nurses, and medical assistants trained in understanding the intention, usage, dosage, side effects, and safety considerations of these medications. Your safety, comfort, and care are their priorities.
Your care team will connect with you prior to your appointment, consultation, and administering the medication. Areas of care that you will discuss include your mental health history, what to expect from Ketamine treatment, billing, and insurance.
Then, you’ll also be scheduled for a consultation with a psychiatrist to determine diagnosis, eligibility, and prepare for your treatment program.
Just before treatment the medical team from the clinic will call you to ensure you know what to expect, discuss the dos & don’ts before & after treatment, and discuss having transportation to and from treatment.
During & After Treatment
During treatment you will meet with a medical assistant, nurse, and your doctor. Your treatment will be administered, and your medical team will check on you periodically before, during, and after to assess how you are feeling physically and emotionally. Ketamine has psychological effects, and physiological effects. Once your treatment is done your care team will ensure you’re feeling well enough to leave the clinic, and will advise you to take it easy for the rest of the day and avoid driving until you’ve had a full night sleep.
Then, if you are also participating in therapy along with Ketamine, you will attend an appointment with your therapist typically within 24-72 hours after treatment.
Consider Your Intention for Treatment
Ketamine is a dissociative anesthetic, and even in dosages aligned for mental health rather than for physical anesthesia, it can produce powerful psychedelic experiences. Psychedelic treatments, including ketamine, induce thoughts and feeling that can be outside of typical daily thinking and processing. For that reason it’s helpful to consider the intention you have going into treatment, and support processing the emotions and experiences post treatment as well.
The psychedelic affect of Ketamine is not only part of the appeal of these medications, but also an aspect of treatment that can have a profound impact. A 2006 John Hopkins study on psychedelic treatments – in the case of this study psilocybin was used – the experience of treatment was marked as one of the most significant experiences of their lives. Additionally studies have shown that ketamine treatment can be particularly effective in treating patients who have both PTSD and treatment-resistant depression concurrently. Given the influence a traumatic experience or experiences have on the persistence nature of challenging mental health conditions, understanding what you want to gain through treatment, and what you wish you heal may be helpful going into treatment.
Pursue a Team Approach with Ketamine Treatment and Therapy
Feelings of overwhelm, and isolation often come with depression, anxiety, and PTSD. It’s important to not only know that you are not alone in your treatment. Therapist who are uniquely qualified to support patients receiving ketamine treatment may be able to support you best.
Intention setting and experience processing can be supported through therapy, and it can be particularly helpful to have someone supporting you in digesting the experience of ketamine therapy after treatment. Perhaps you’re thinking, “Whoa, won’t I be too ‘out of it’ to navigate therapy during or immediately after treatment?”
The answer to that question, for you, might be yes.
We have found that not everyone feels up to the task of in-depth conversation during or immediately after treatment. However, this isn’t necessarily an issue. You’re still receiving benefit of ketamine treatment after the dissociative and psychedelic affects have worn off.
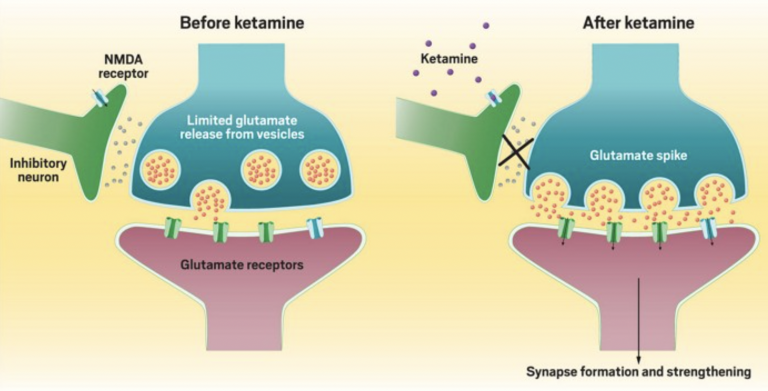
Ketamine is thought to support a brain change concept called neuroplasticity. This refers to the brain’s ability to reorganize synaptic connections – sort of like a software update on your computer. Studies have shown that there may be optimal windows of time, after the dissociative effects of ketamine are gone, to take advantage of the change-making aspects of the treatment. Therapists who are well-versed in ketamine’s ability to treat mental health and specialize in supporting individuals who have experienced trauma, or have hard to treat or treatment-resistant disorders can offer relevant can offer guidance that positively impacts healing.
Bottom line – mental health healing can be a team-effort, and a Therapist is an important member of the team who will continually help you focus your needs, experiences, and healing at the center of care.
“My advice to anyone anxious when starting therapy is to approach it with an open mind,” Ken shares, a therapist at Heading.
In other words, it’s important to adopt a more flexible attitude towards your own general beliefs about therapy and mental health, and even ketamine treatment.
If you are receiving Ketamine and also attending therapy your therapist will continue to guide you with warmth and compassion, and they’ll be able to do so more effectively if you are open about what treatments you are seeking, and if they are specialized in supporting patients who are attending both psychedelic therapy and talk therapy concurrently.
Want to find out if Heading is right for you?
Complete our consultation form and an intake specialist will get in touch.



 Over the past several years,
Over the past several years, 
 condition, and so on. With all these expectations rolling around in your head as you prepare for therapy, it’s natural to feel anxious.
condition, and so on. With all these expectations rolling around in your head as you prepare for therapy, it’s natural to feel anxious.


 I’ve always struggled to get myself to try new things. I like consistency and predictability, and new experiences get in the way of maintaining my desired level of stability.
I’ve always struggled to get myself to try new things. I like consistency and predictability, and new experiences get in the way of maintaining my desired level of stability.
 As the hol
As the hol #2 Volunteer or Donate to a Charity
#2 Volunteer or Donate to a Charity

 #9 Go Somewhere That’s Normally Too Busy
#9 Go Somewhere That’s Normally Too Busy

 When people experience grief, they may not outwardly make their feelings known. It can be difficult to know exactly what to say and easy to interpret someone’s silence as “ok-ness.”
When people experience grief, they may not outwardly make their feelings known. It can be difficult to know exactly what to say and easy to interpret someone’s silence as “ok-ness.” 















 Over the past few years, psychedelics such as LSD and psilocybin mushrooms have garnered much attention as researchers explore their potential use in treating mental health conditions.
Over the past few years, psychedelics such as LSD and psilocybin mushrooms have garnered much attention as researchers explore their potential use in treating mental health conditions.  Though there is much disagreement about what counts as a psychedelic, it’s generally accepted that they must induce specific mind-altering effects. Some argue this is all that is required. In other words, they claim that as long as the substance causes a “psychedelic experience,” then it’s a psychedelic.
Though there is much disagreement about what counts as a psychedelic, it’s generally accepted that they must induce specific mind-altering effects. Some argue this is all that is required. In other words, they claim that as long as the substance causes a “psychedelic experience,” then it’s a psychedelic. 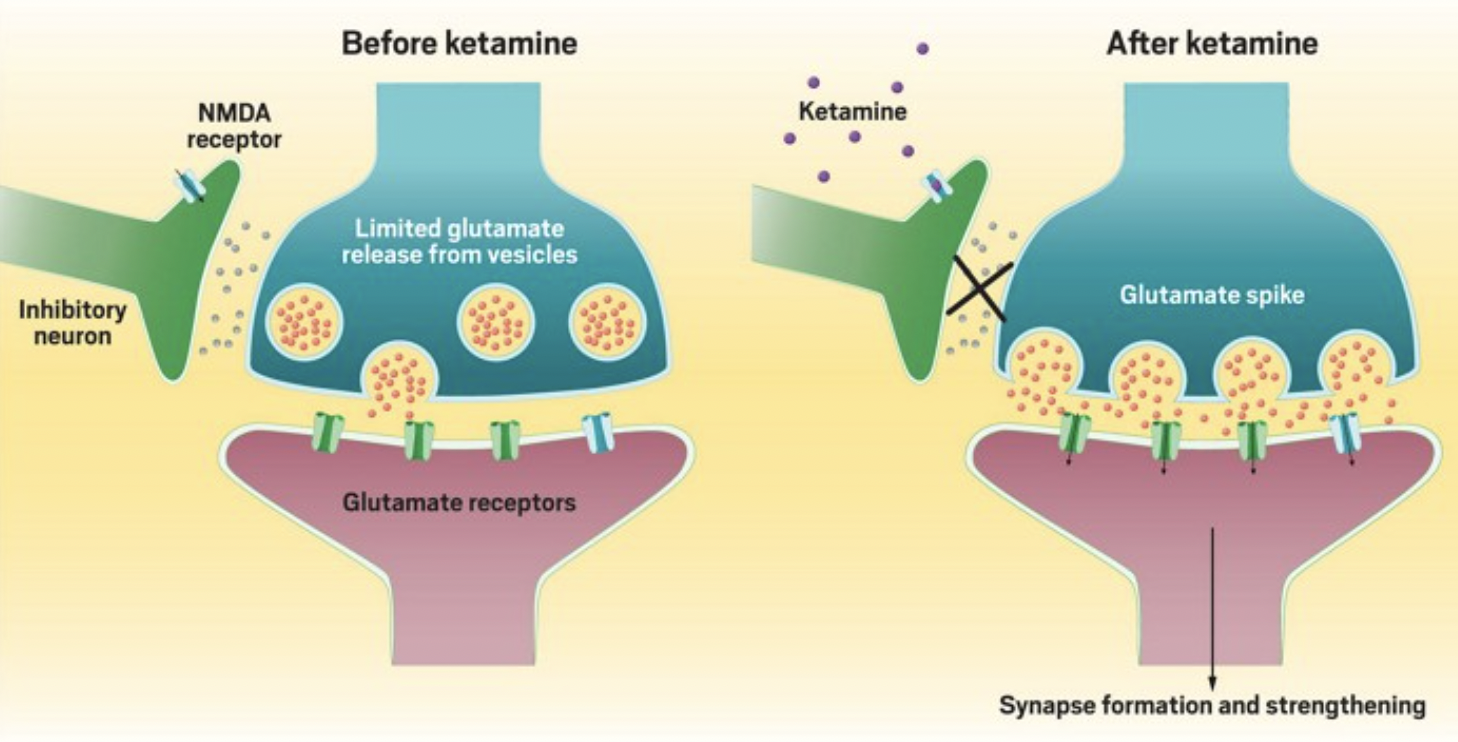


 What are They Made Of?
What are They Made Of? 


 Between coffee, tea, soft drinks, and energy drinks, caffeine is one of the most commonly consumed psychoactive drugs.
Between coffee, tea, soft drinks, and energy drinks, caffeine is one of the most commonly consumed psychoactive drugs.