Mental Health Care Lags in Rural Texas. Can Teletherapy Help Now?
According to Mental Health Texas, more than three million adults in Texas have a mental health condition. For those in rural areas, adequate mental health care is hard to come by. For example, there isn’t a single hospital in 28 percent of the state’s counties. Even when those in need can make the trek crisis center, hospitals often lack the resources to treat them.
This overall lack of access can have serious consequences as Texans wait to receive or completely forgo treatment. When it comes to mental health care, time is of the essence. Delayed treatment is associated with a wide range of adverse outcomes, from a lower likelihood of remission to cognitive impairments to an increased risk of suicide.
Advocates Propose Solutions to Lawmakers
Mental health advocates have been discussing potential solutions with Texas lawmakers. One of the more glaring issues with the mental health system for rural Texans is the lack of crisis centers. “As I’ve traveled around the state, I have seen the need,” shares Lt. Gov. Dan Patrick. “We don’t have a mental health facility in the Panhandle, so I’m proposing we build one there. This is something we have to do for our communities.” Lt. Patrick is also asking for more hospital beds in several locations, including 300 more in Wichita Falls and Terrell and 140 more in the Rio Grande Valley.
“While some hospitals need more beds, others have more than they can fill.” Lt. Patrick suggests this is mainly due to nursing staff shortages.
“There simply aren’t enough mental health professionals to care for a full house of patients.” He says, “That’s why, in addition to more beds, advocates are calling for tuition assistance to get more students into nursing school and pay raises to incentivize them to take the jobs that are out there.”
Getting more students into nursing programs is a big step in the right direction. Still, according to Dr. Steve Bain, founding director of the Institute for Rural Mental Health Initiatives, we also need to focus on the nursing curriculum. For example, he suggests that there should be more opportunities for nursing students to finish their fieldwork in rural communities.
“We’ve got to be constantly connected with these communities,” shares Dan. “It’s going to take research and research funding. And it’s going to take putting our graduate students who need their practicum and internships into these rural communities.”
The Role of Teletherapy
New buildings, beds, and updated nursing programs are a critical part of a comprehensive mental health care system in rural Texas, but what can you do if you need help now?
 Over the past few years, as safety precautions made many in-person services infeasible, we saw a dramatic and sustained rise in the use of telehealth services, including teletherapy and telepsychiatry. According to a Zocdoc report, 87 percent of mental health visits were virtual in May 2022.
Over the past few years, as safety precautions made many in-person services infeasible, we saw a dramatic and sustained rise in the use of telehealth services, including teletherapy and telepsychiatry. According to a Zocdoc report, 87 percent of mental health visits were virtual in May 2022.
Virtual mental health services have remained popular for reasons which suggest they can help improve mental health care in rural Texas. Telemental health makes mental health care more accessible. But it does in many different ways that remove the obstacles to care for those in need outside of the urban areas of Texas.
Eliminates the Need to Travel Far
Given that in rural Texas, mental health centers are few and far between, distance and travel times are likely significant factors preventing many from seeking care. With teletherapy, there’s no need to travel anywhere.
Patients Don’t Have to Take Time Off
As travel time increases, so does the amount of time one needs to take off work for an appointment. According to the report, 56 percent enjoyed not having to take time off work or responsibilities to travel to appointments.
More Affordable
Not having to take time, or as much time, away from work to attend appointments is not only convenient it is also addressing cost concerns of hourly and shift workers. 1 in 4 Americans already cite cost concerns as a significant reason for avoiding medical appointments. Missing work for an appointment compounds the financial strain.
Telehealth options make it easier for appointments to occur outside of standard work hours which is a more convincing proposition for those who don’t work a traditional 9 to 5.
Without the need to pay for transportation or take time off, it’s not surprising that telemental health is easier on the wallet.
Provides Patients with a Better Selection of Mental Health Professionals
Because you can pick providers from a larger area, you typically have a much bigger selection of professionals when booking a virtual appointment. This makes it easier to find the right therapist. For example, it can help find a provider who works with your insurance, specializes in your mental health needs, matches up with your cultural background, speaks your language, or simply vibes with you in a way that enhances your therapy journey.
Gets Rid of Physical Barriers
Teletherapy allows those who otherwise could not make it to an in-person appointment due to physical disabilities. For example, mental health professionals working out of their own homes may not set up the proper accommodations to make their practice equally accessible for individuals of all abilities. With some estimates suggesting that nearly one in five farmers has a disability that interferes with their ability to perform their job, this barrier may be causing many Texans to avoid receiving care.
Reduces the Problem of Stigma
Though the public perception of mental health has improved significantly, there is still a considerable amount of stigma associated with having a mental health condition and seeing a therapist. This can be a bigger obstacle in rural areas.
“Stigma, cultural norms, the power of the grapevine in rural communities where folks don’t want other people to know when they’re accessing services…all these factors contribute to a large portion of rural residents not getting help when they need it,” shares Dr. Carly McCord, director of Telebehavioral Health and clinical assistant professor at Texas A&M University College of Medicine
Virtual mental health care makes this less of an obstacle, as patients don’t have to go out in public or risk being identified. Telemental health offers them greater privacy and shields them from some of the effects of stigma.
Can Teletherapy Help With Crisis Situations?
Many of the updates that mental have advocates are lobbying for are designed to help those in crisis situations. While teletherapy can help increase access to mental health care in general, one may wonder whether it can do much to help those in the middle of a mental health crisis.
One straightforward way teletherapy may help is by preventing the circumstances that require a mental health facility from arising in the first place. Access to regular visits with a mental health professional makes it less likely that one’s mental health condition or circumstances worsen to the extent that crisis intervention is necessary. Since teletherapy allows more patients to see therapists and may increase the odds that they continue to see their provider regularly, it can serve as a preventative measure.
With that said, many crisis-specific interventions aren’t available through teletherapy, meaning mental health centers with in-person treatments will remain a crucial component of Texas’s comprehensive rural mental health system.
Takeaway
For many Texans in rural areas, there are limited mental health resources. From distant crisis centers to understaffed hospitals, finding care when you need it can be challenging, if not impossible.
Mental health advocates aim to change this. They have proposed a variety several changes to lawmakers, including:
- Adding more mental health facilities
- Increasing the number of beds
- Covering nursing tuition and offering pay raises
- Updating nursing programs to include more practicums in rural areas
Telehealth is also an essential part of the solution to creating a comprehensive mental health system for rural texas. Its popularity has risen significantly over the past few years for good reasons. Specifically, teletherapy can help Texans in rural areas with unmet mental health needs access adequate care because it:
- Eliminates the need to travel
- Helps patients get care without taking time off
- Makes care more affordable
- Provides a larger selection of mental health professionals
- Gets rid of physical barriers
- Reduces the problem of mental health stigma

Want to find out if Heading is right for you?
Complete our consultation form and an intake specialist will get in touch.




 Stress is generally seen as an undesirable state to be avoided whenever possible. It feels bad, can interfere with attention and productivity, and, when experienced chronically, may harm the body and lead to mental illnesses, including depression and generalized anxiety.
Stress is generally seen as an undesirable state to be avoided whenever possible. It feels bad, can interfere with attention and productivity, and, when experienced chronically, may harm the body and lead to mental illnesses, including depression and generalized anxiety. 
 Stress Can Enhance Your Memory
Stress Can Enhance Your Memory Memory is a good example of this. Animal studies show the brains of mice that underwent a stress test grew new neurons and performed better on learning and memory tests.
Memory is a good example of this. Animal studies show the brains of mice that underwent a stress test grew new neurons and performed better on learning and memory tests.  Perhaps more surprising than the beneficial effects of stress on the mind are its healing effects on the body. While we can get an intuitive sense of how stress might help us prepare for danger or feel extra motivated to complete tasks, it’s a little harder to see how it might benefit us at a biological level.
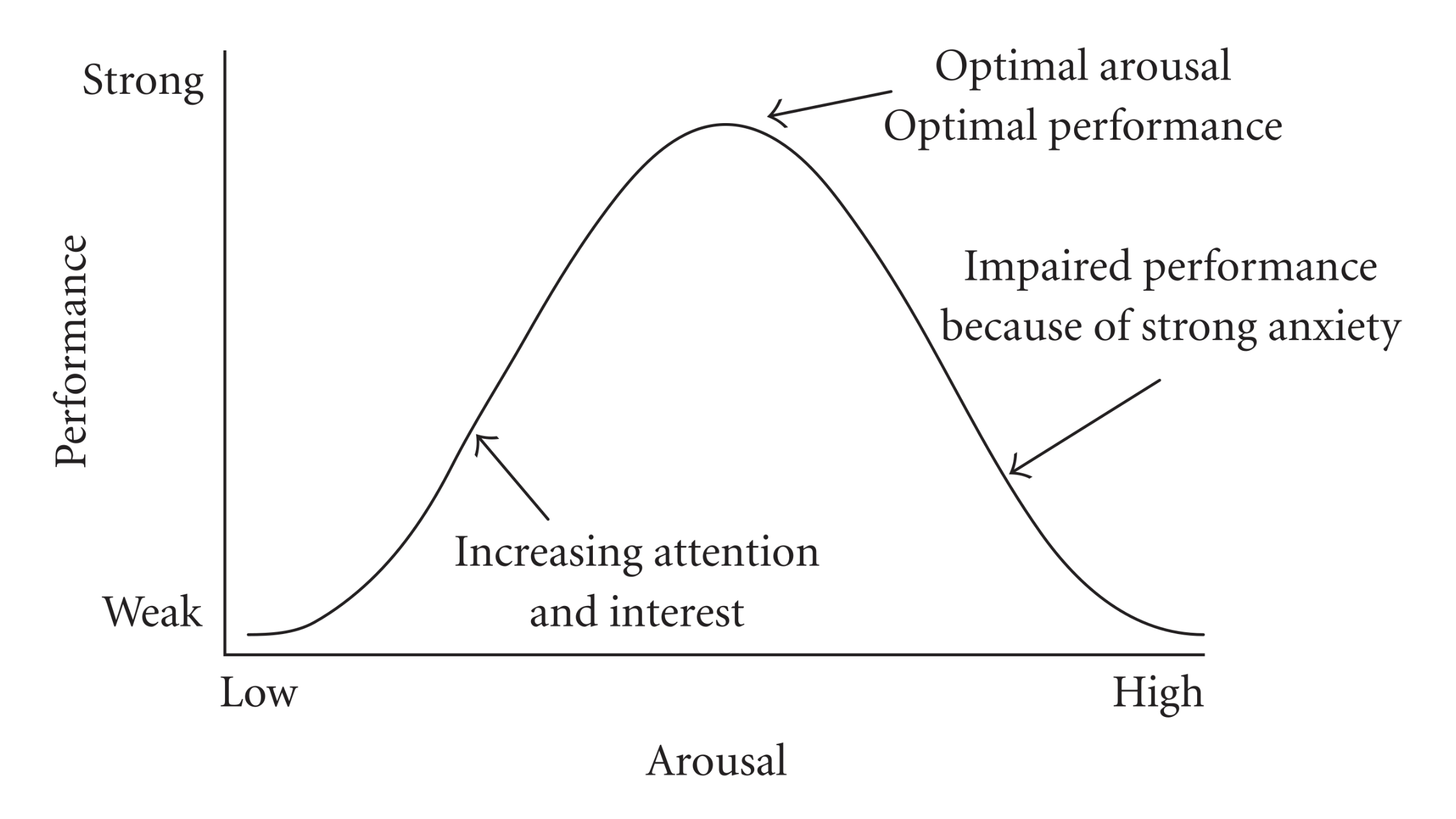
Perhaps more surprising than the beneficial effects of stress on the mind are its healing effects on the body. While we can get an intuitive sense of how stress might help us prepare for danger or feel extra motivated to complete tasks, it’s a little harder to see how it might benefit us at a biological level. As we learned from the Yerkes-Dodson Law, some stress is necessary for optimal performance. But how much is suitable for any person depends on various factors from skill level to personality to confidence. So how much is enough for you?
As we learned from the Yerkes-Dodson Law, some stress is necessary for optimal performance. But how much is suitable for any person depends on various factors from skill level to personality to confidence. So how much is enough for you? 

 both with and without medications had comparable improvements in their symptoms.
both with and without medications had comparable improvements in their symptoms. 
 Every year an estimated 800,000 U.S. adults make New Year’s resolutions in the hopes of improving their lives and developing healthier habits.
Every year an estimated 800,000 U.S. adults make New Year’s resolutions in the hopes of improving their lives and developing healthier habits. This is a perfectly normal reaction, and it’s important not to judge yourself if you’ve gone a little off course. “Guilt and shame will only serve to keep you from making progress,
This is a perfectly normal reaction, and it’s important not to judge yourself if you’ve gone a little off course. “Guilt and shame will only serve to keep you from making progress, Your journey to mental wellness will almost certainly require you to make some internal changes.
Your journey to mental wellness will almost certainly require you to make some internal changes. 
 Once you’ve made the brave step of making an appointment with a therapist, you may wonder, “what am I setting myself up for?” Knowing what to expect can help alleviate any anticipatory anxiety and prepare you for your first session.
Once you’ve made the brave step of making an appointment with a therapist, you may wonder, “what am I setting myself up for?” Knowing what to expect can help alleviate any anticipatory anxiety and prepare you for your first session. 

 After you’ve come down from your first session, you may have a bit of homework to do. Therapy doesn’t just happen within the walls of your therapist’s office, and they may want to get you started before your next session. This will likely involve something light at first. You may be asked to try practicing mindfulness or write some quick journal entries when you encounter something that triggers anxiety or low mood.
After you’ve come down from your first session, you may have a bit of homework to do. Therapy doesn’t just happen within the walls of your therapist’s office, and they may want to get you started before your next session. This will likely involve something light at first. You may be asked to try practicing mindfulness or write some quick journal entries when you encounter something that triggers anxiety or low mood. 


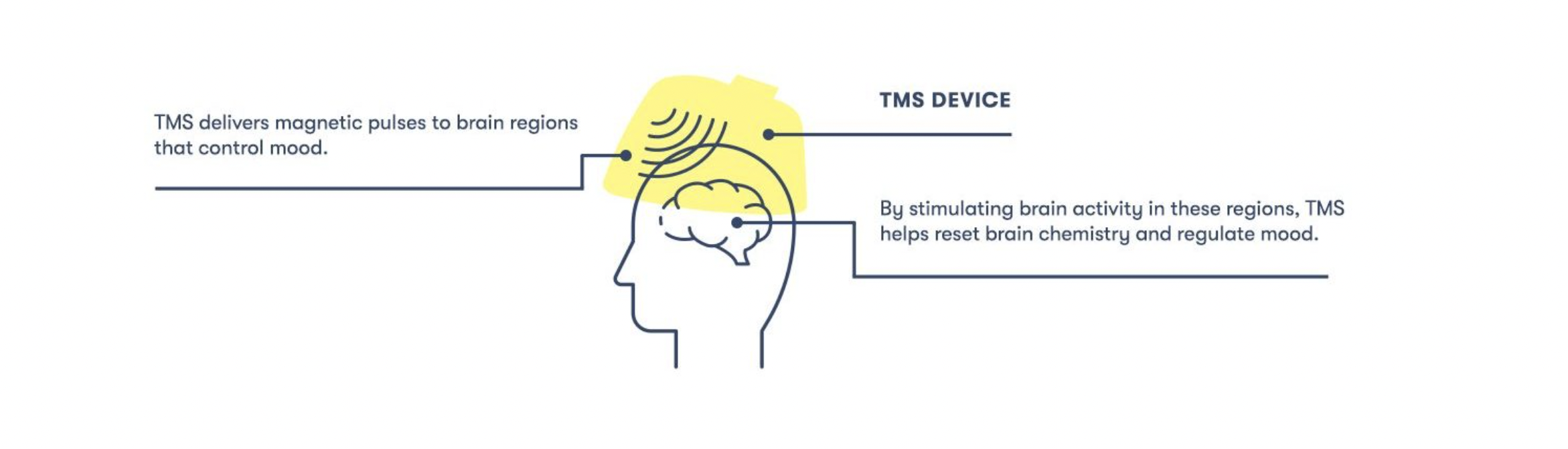
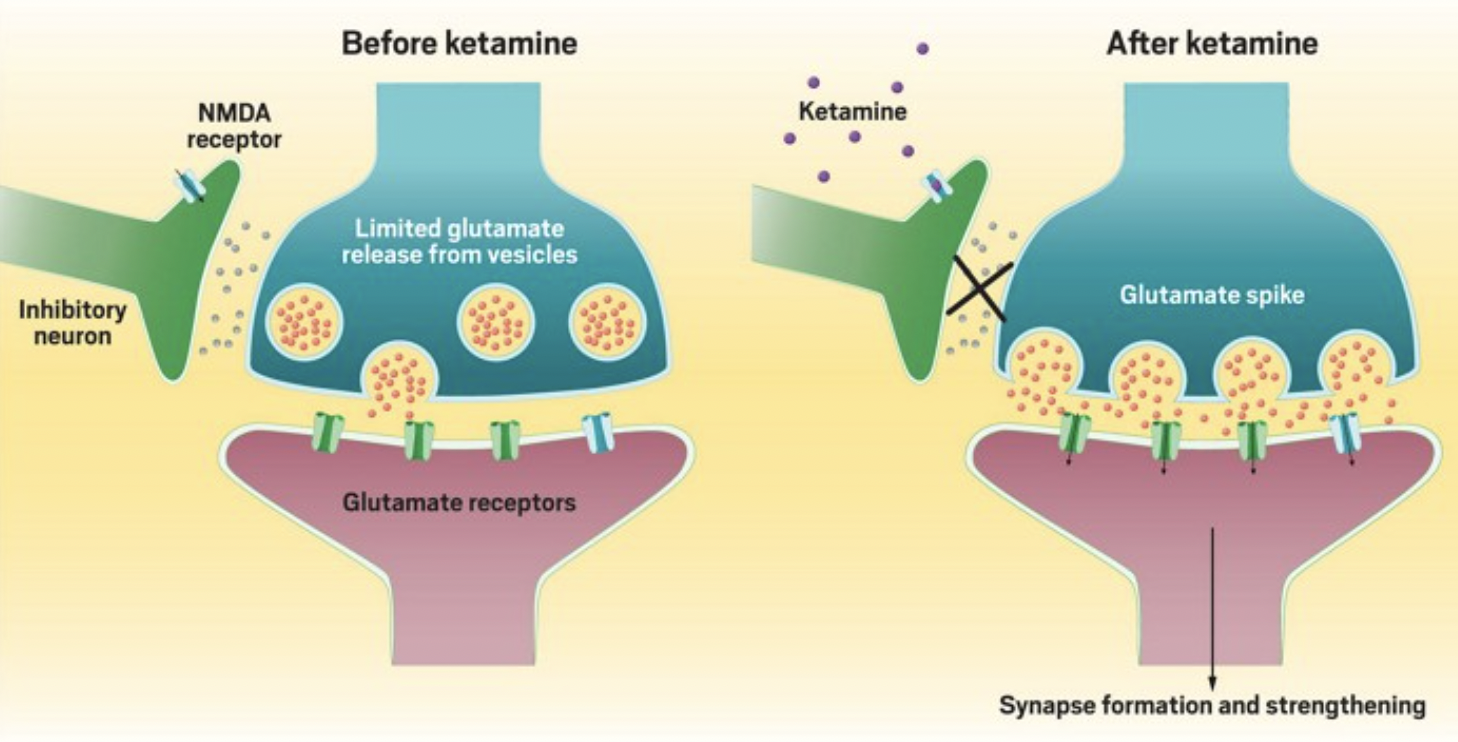
 changes are associated with better therapeutic outcomes. For example, ketamine appears to
changes are associated with better therapeutic outcomes. For example, ketamine appears to 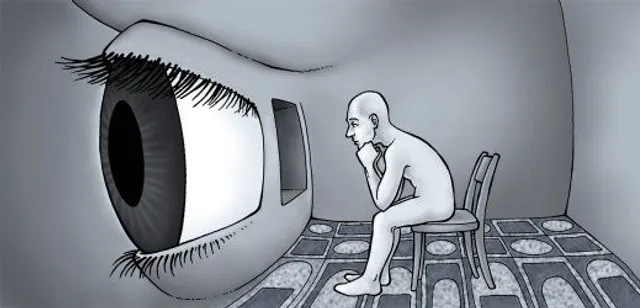











 I’ve always struggled to get myself to try new things. I like consistency and predictability, and new experiences get in the way of maintaining my desired level of stability.
I’ve always struggled to get myself to try new things. I like consistency and predictability, and new experiences get in the way of maintaining my desired level of stability.
 As the hol
As the hol #2 Volunteer or Donate to a Charity
#2 Volunteer or Donate to a Charity

 #9 Go Somewhere That’s Normally Too Busy
#9 Go Somewhere That’s Normally Too Busy