Sugar, Mood, and Mental Health: Interview with a Nutritional Therapist
The holiday season is a time of gatherings, gifts, and of course, a gluttonous indulgence in sweet treats.
While some sugar consumption is perfectly normal and healthy, a high-sugar diet, even temporarily, can negatively impact one’s mood and mental health. As a result, it’s important to be mindful of your sugar intake during the holidays and as you carry on afterward with your regular diet.
To learn about sugar’s connection with mood and mental health and how to adopt healthier habits, we sat down with Austin, Texas-based Registered Dietician Nutritionist Sally Twellman. She is our in-house nutritional therapist here at Heading Health, and she shared experience supporting mental health treatments with dietary and lifestyle changes.

Q & A with Sally Twellman RDN, LD
Are Sugar Rushes and Crashes Real? If So, What Causes Them?
Yes, for sure, and this goes for carbohydrates in general. When we have a large amount of carbohydrates, our blood sugar rises rapidly, which causes an equally sharp increase in insulin. This increase in insulin causes a rapid drop in blood sugar, and that’s when you get that slump, which can make you feel tired, lethargic, and even a little bit irritable. In turn, this can cause sugar cravings and, ultimately, a vicious feedback loop of sugar consumption followed by a crash followed by more sugar consumption, and so on.
Are There Long-Term Mental Health Consequences of a High-Sugar Diet?
Very much so.
For example, a high-sugar diet is correlated with depression. One of the many ways it might contribute to depression is through frequent and erratic fluctuations in blood sugar levels. Some fluctuations are normal, but when the peaks become too large and too frequent, it is very stressful for the body and can contribute to chronic inflammation, which is associated with adverse mental health outcomes.
Another way that having a lot of sugar in your diet can impact mental health is through its connection with diabetes. Over time, people who eat a carbohydrate-heavy diet are disproportionately more likely to develop insulin resistance, predisposing them to depression.

The third way having lots of very sugary foods can impact mood is that it changes the gut microbiome. Your body adapts to whatever you eat, and if you mostly eat high carbohydrates and low-fiber foods, the bacteria you will grow more of will be the kind that thrives in that environment. And those bacteria are typically not the ones that are beneficial for maintaining good neurotransmitter production, which your brain needs to send messages chemical messages and, ultimately, to produce good feelings.
Is the Damage Reversible?
Yes. Even a dietary change of two weeks to a Mediterranean-based diet, for example, can have a profoundly positive impact on your gut microbiome. This means that if you’re experiencing a low mood resulting from a high-sugar diet, it’s possible to undo the damage and experience benefits after just a few weeks on a low-sugar, high-nutrient diet.
Does the Sugar Source Matter?
Absolutely. The source matters for a variety of reasons. For one thing, some sources make it much easier to consume lots of sugar than others, which is why I highly recommend people avoid sugar-sweetened beverages. We don’t really get that fullness factor like we do when we eat the same amount of sugar or calories in, say, a cookie. So, we can consume a lot of sugar just by drinking regular amounts of liquid without realizing it.

Also, some sugar sources contain ingredients that help to balance out the sugar and help our bodies break it down. Protein, fiber, and fat are good examples. When sugar comes from a source with sufficient amounts of fat or protein, it’s released incrementally into your bloodstream, which helps to avoid the kind of spikes and dips that are particularly unhealthy. So, if you want a cookie, try having it alongside some yogurt with protein and fat to help balance out your blood sugar.
Does the Type of Sugar Matter (e.g., Glucose vs. Fructose)?
In theory, it should matter because our liver is what’s primarily responsible for breaking down fructose. So, part of why food and drinks containing high fructose corn syrup are dangerous is because they can cause the liver to overwork, resulting in all sorts of problems. For example, nonalcoholic fatty liver disease can be caused by a high carbohydrate diet and insulin resistance. Over time, a fatty liver becomes inflamed, which can cause inflammation throughout the body, which, again, is associated with adverse mental health outcomes.
Is Fruit Okay?
You might think, “well, I shouldn’t eat fruit because fruit is high in sugar fruit and it’s high in fructose, which is harder to process,” but naturally occurring fructose isn’t the same as high fructose corn syrup. It’s also coupled with fiber and many other nutrients your body needs to break it down. So, for example, your body can break down the amount of sugar and carbohydrates in an apple in a healthy way because it also comes with things like magnesium and fiber, which it needs to support the good bacteria that help process sugar. So, fruit is not bad. It’s separate from things like gummy bears and other high-fructose snacks.


What About Artificial Sweeteners?
I’m not a fan of artificial sweeteners. They have been linked to things like migraines and changes in the microbiome, and they have to be detoxified by our overworked livers.
Also, even though artificial sweeteners have zero calories, they can still cause an increase in insulin. This is because part of what causes your body to release insulin is the sweet taste of sugar on your tongue.
Whenever you have something sweet, your brain will send signals down to your pancreas saying, “something sweet’s coming down. You better start pumping up insulin.” As a result, your insulin levels will increase, and these spikes can be just as significant as they would be with natural sugar.
So, if you feel like you need to add some sweetness to your beverages, try more natural sweeteners like honey and maple syrup. These may not taste as sweet as table sugar, but over time your taste preferences will adjust to the lower sweetness levels. Another option is to add natural sugar alternatives, like monk fruit or stevia if you like those.
You might think, “well, I shouldn’t eat fruit because fruit is high in sugar fruit and it’s high in fructose, which is harder to process,” but naturally occurring fructose isn’t the same as high fructose corn syrup. It’s also coupled with fiber and many other nutrients your body needs to break it down. So, for example, your body can break down the amount of sugar and carbohydrates in an apple in a healthy way because it also comes with things like magnesium and fiber, which it needs to support the good bacteria that help process sugar. So, fruit is not bad. It’s separate from things like gummy bears and other high-fructose snacks.
What’s a Good Tip for Managing Our Sugar Intake During the Holidays?
My basic recommendation is to be picky about the added sugar you take into your diet. As the holidays continue, it’s important to choose things that you thoroughly enjoy, like really delicious cookies or a great pie. Don’t waste it on sweethearts (unless you really like those, of course). It’s also best to choose something with nutritional value, like dark chocolate, which has antioxidants.
What’s the Best Way to Get Off of a High-Sugar Diet?
The best way is just to go cold turkey. Weaning yourself off incrementally by decreasing the amount of sugar you add to your coffee is generally less effective. Because you get such a robust physiological reward when you have sugar, your body will want more, and you’ll have to endure intense sugar cravings every time. So, it’s best to tough it out for a little while, and you will begin to crave it less.
People in Austin, Texas as well as Texans across the state connect with Sally to supplement their mental health care with nutritional support. Those interested in working with Sally are encouraged to reach out to Heading to set up a consultation.
Want to find out if Heading is right for you?
Complete our consultation form and an intake specialist will get in touch.




 dderall, Ritalin, and Concerta are the standard treatments for ADHD. These medications work by increasing chemical messengers called dopamine and norepinephrine in the brain’s central nervous system. While highly effective, these medications aren’t the best choice for everyone. Some individuals have other conditions that stimulants can exacerbate, such as:
dderall, Ritalin, and Concerta are the standard treatments for ADHD. These medications work by increasing chemical messengers called dopamine and norepinephrine in the brain’s central nervous system. While highly effective, these medications aren’t the best choice for everyone. Some individuals have other conditions that stimulants can exacerbate, such as: Decrease distractions: Make a point to limit easy distractions. Make a list of common distractions and avoid them while working on important tasks. Some common anti-distraction strategies may include setting your phone and computer to do-not-disturb mode and avoiding working around your TV.
Decrease distractions: Make a point to limit easy distractions. Make a list of common distractions and avoid them while working on important tasks. Some common anti-distraction strategies may include setting your phone and computer to do-not-disturb mode and avoiding working around your TV.  Aside from diet, exercise has been investigated as a potential tool for alleviating the symptoms of ADHD. For example, a recent
Aside from diet, exercise has been investigated as a potential tool for alleviating the symptoms of ADHD. For example, a recent 
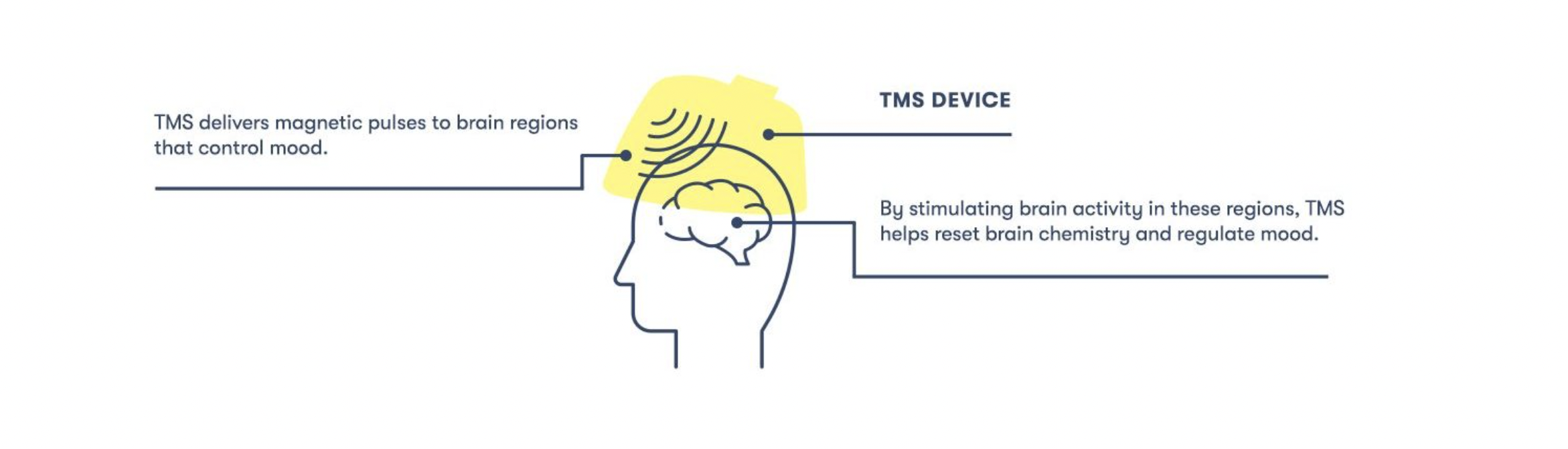
 One of the ways we accomplish this with TMS is with the Magstim StimGuide, the first navigational system specifically designed for the clinical market. After the target location has been identified, the StimGuide stores the location using four distinct parameters captured by a 3D snapshot of the treatment area. When administering TMS, this tool helps practitioners consistently identify the target area by emitting a green light when all four parameters are aligned.
One of the ways we accomplish this with TMS is with the Magstim StimGuide, the first navigational system specifically designed for the clinical market. After the target location has been identified, the StimGuide stores the location using four distinct parameters captured by a 3D snapshot of the treatment area. When administering TMS, this tool helps practitioners consistently identify the target area by emitting a green light when all four parameters are aligned.