What's Does Spravato Feel Like? A Patient's Perspective
This post was written by a member of our team currently receiving treatment, using Spravato, in Michigan where he resides. He wanted to share his story with us in hopes that it might help patients seeking care with Heading. While he is not a patient of Heading (as Heading provides care to patients in Texas) his treatment program, environment, and experiences detailed in his share are very similar to those at Heading. We are grateful he chose to share his story with us.

I have suffered from anxiety and depression for most of my life. Treatment began at age 12 when I was diagnosed with generalized anxiety and obsessive-compulsive disorder (OCD). While the initial treatments helped to some degree, many symptoms remained, and the side effects of the drugs I took became intolerable.
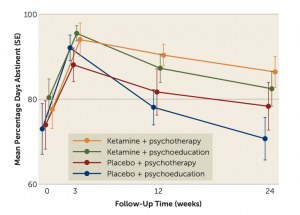
Over the next 17 years, I switched from one oral antidepressant to the next, desperately trying to find something that addressed my symptoms without causing side effects that were worse than what I was trying to treat. Eventually, my psychiatrist recommended a drug called Spravato (esketamine nasal spray), a rapid-acting drug used for treatment-resistant depression. He told me that Spravato works differently than traditional antidepressants by increasing levels of glutamate and brain-derived neurotrophic factor (BDNF). These two changes have been associated with improvements in depression and anxiety. Knowing this, I felt hopeful that I might get the benefits I was looking for without the drawbacks I was trying to avoid.
Though I was excited about trying out the new intervention, I grew increasingly anxious as I awaited my first treatment session. Both esketamine (the active ingredient in Spravato) and its more famous cousin, ketamine, are psychoactive, meaning they can alter one’s normal state of consciousness, affecting one’s thoughts, feelings, and perceptions.
Before trying Spravato, I had very little experience with psychoactive drugs and none with anything that might be considered a psychedelic. As a result, I had no idea what to expect. To make matters worse, I felt that I wouldn’t react well to the experiences that Spravato might bring about because I suffered from severe anxiety. I went into my appointment blind to what I was about to experience. Though my fears were unwarranted, I would have benefited greatly from a clear and honest description of what was to come.
My Experience with Spravato
Below I describe to the best of my ability what I typically feel during a Spravato treatment session. Though some of these experiences may generalize, it’s important to remember that everyone’s brain is unique and may react differently to Spravato.
Dissociation
One of the more talked about effects of Spravato is its ability to cause dissociation. Though it is described differently by different people, the effect is generally characterized as a temporary feeling of disconnection from one’s thoughts and feelings.

I like to describe my personal experiences with dissociation as akin to the sensation one gets when looking at their avatar through a virtual reality headset. Everything is in the location it’s supposed to be and moves when it should, but you don’t identify with your avatar. Its movements don’t feel like your movements. Its body doesn’t feel like your body.
The feeling of separation from my thoughts is harder to describe. The best I can say is that it feels like I am “viewing” my thoughts rather than “thinking” them. They simply pass by, unauthored by me.
Feeling of Relaxation
Despite having unusual sensations like the feeling of dissociation, I often experience a wave of relaxation as my concerns and worries drift away. My thoughts quiet down, and former troubles begin to feel like they don’t matter as much.
Feelings of Stress and Anxiety
Though Spravato can be pleasurable, it can also be unpleasant and stressful. I believe this is at least partially the result of the following two factors.
First, while under the effects of Spravato, my mind tends to focus on unpleasant thoughts at the core of many of my worries (more on this below). Though these thoughts are easier to entertain at the time, they can still be challenging to confront.
Second, aside from its psychological or psychoactive effects, Spravato causes physical sensations that tend to be more unpleasant. For example, I often get dizzy and feel like I am slowly spinning in my chair. As a result, I feel nauseous. When these sensations become too intense, the overall experience can become quite stressful. Fortunately, my doctor prescribed an antiemetic (i.e., an anti-nausea drug), so these sensations have become less frequent and more tolerable.
Increased Empathy

The state that Spravato puts me in makes it easier for me to put myself in other peoples’ shoes. Often, I will spend time thinking about past arguments or disagreements. While doing so, I have an easier time understanding where the other person was coming from and why their reactions and feelings were appropriate. More generally, I tend to have a stronger concern for the well-being of others.
Enhanced Ability to Confront Unpleasant Thoughts
Through my Spravato experiences, I have realized that at the heart of many of my daily fears are more general worries that I have trouble recognizing or confronting. While under the effects of Spravato, my attention is almost unavoidably directed toward these fundamental concerns
Here’s a personal example to shed light on how this works. Among the many things I worry about, work is often at the top of the list. I worry while working on assignments, submitting them, waiting for feedback, etc. Though I had spent so much energy feeling anxious about this, I never looked at the underlying concern or belief that connected all these more specific worries. During one Spravato treatment, I realized that I had deep concerns about my intellectual abilities and that I viewed each work assignment as a potential instance where my real lack of capability would be revealed.
Though the fear remains, knowing it exists and is responsible for so many other specific worries has made it easier to deal with.
Visual Distortions
Around 10 minutes into each treatment, I start to notice some visual effects. First, my vision becomes fuzzy, and I have trouble refocusing each time I move my eyes. Over the next few minutes, this effect increases in intensity until everything looks as though it is shaking for a few seconds after I shift from looking at one spot to another.
Aside from becoming fuzzier and shakier, my vision tends to change in a different way. Specifically, objects appear to be slowly expanding and contracting as if they are breathing. Often, I’ll try to match my breath to the rate at which the things are “breathing.” It’s pretty relaxing.
When I close my eyes, I notice a further visual effect. As I keep them shut, I see faint geometric patterns. This is especially noticeable when my eyes are almost but not completely closed, which happens to me somewhat frequently when dozing off under Spravato. My guess is that my brain is doing its best to interpret the unusual visual stimuli it is getting, and the result is that I have some minor closed-eye visuals.
Post-Treatment Effects
Though many of the effects subside by the end of the two-hour treatment, some remain for several hours. I tend to feel tired, off-balance, and a bit groggy. These effects slowly dissipate as the day goes on but do not linger into the next day.
Concluding Thoughts
From enhanced empathy to feelings of dissociation, Spravato experiences can feel intense or overwhelming when you don’t know what to expect. After I learned first-hand what the experience feels like, my Spravato sessions became much more relaxing and pleasant. Hopefully, my descriptions will help other anxious patients get there more quickly.
Stay tuned for part two of this blog, where I describe the long-term effects of Spravato on my depression and anxiety.
Want to find out if Heading is right for you?
Complete our consultation form and an intake specialist will get in touch.